What is genetic testing?
Genetic testing is a type of medical test that looks for changes, called pathogenic variants, in ones DNA. Genetic testing is useful in many areas of medicine and can change the medical care the patient or its family member receives. For example, genetic testing, such as the one provided by Cogentech, can provide information about the risk to develop cancer.
Genetic testing is voluntary. Because testing has benefits as well as limitations, the decision about whether to be tested is a personal and complex one. A medical geneticist or genetic counselor can help by providing information about the pros and cons of the test and discussing the social and emotional aspects of testing. In most European countries genetic counseling is mandatory and recommended by the professional guidelines.
In the context of genetic testing for hereditary tumors, a positive testing outcome will influence the screening protocol and possible preventive measures that a doctor will recommend.
What is a hereditary tumor?
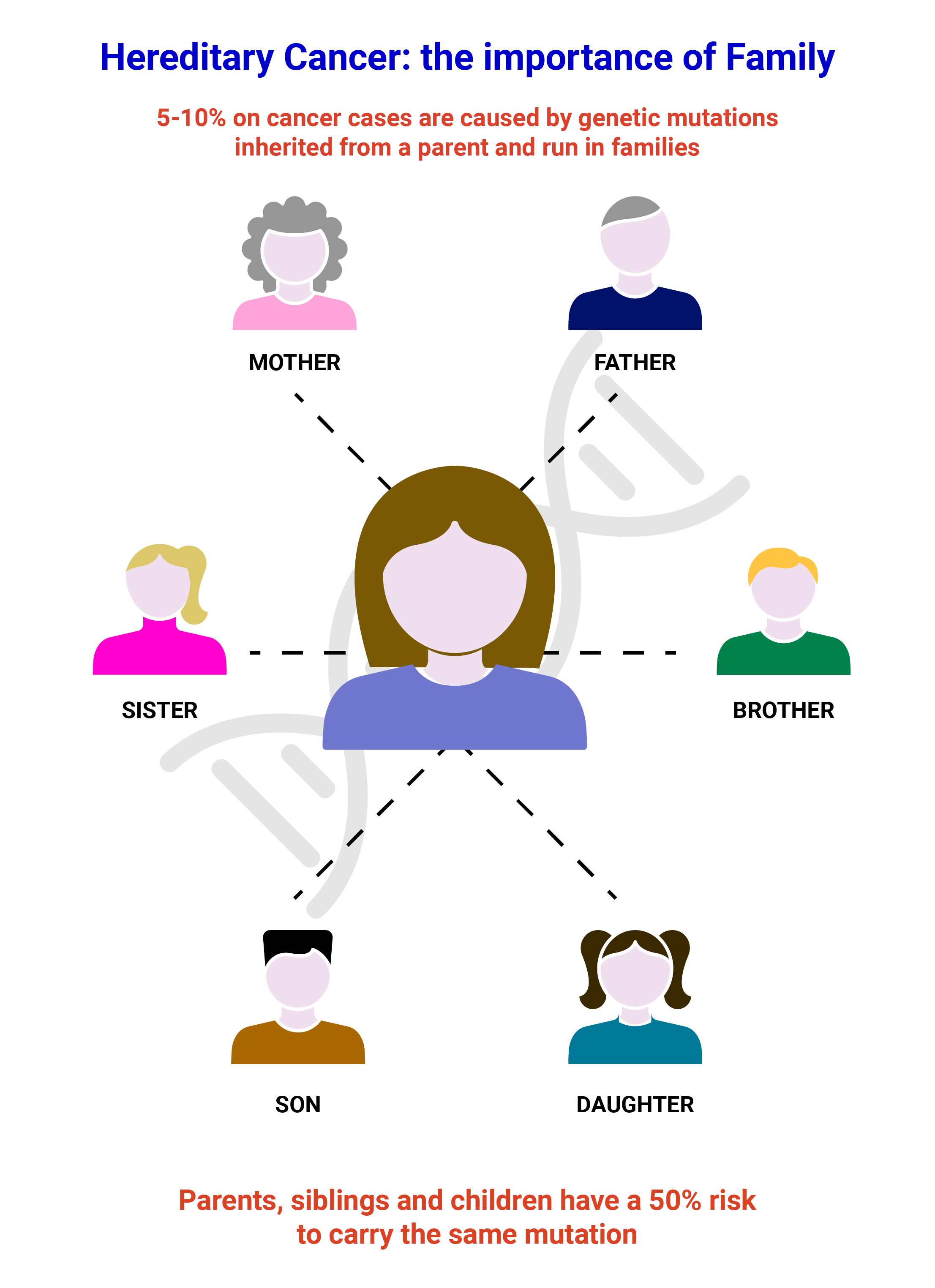
A hereditary tumor is a type of cancer caused by mutations in ones genes which are passed from generation to generation. Hereditary tumors account for 5-10% of most cancers, but some cancers are more likely to be hereditary, such as ovarian cancer (20-25%). Carrying a mutation in a gene known to be linked to hereditary cancer may cause a higher-than-average risk of developing certain types of cancer. In families with hereditary cancer, cancers are often diagnosed at young ages. In addition, family members might develop the same or related cancers, and some family members may develop more than one separate type of cancer. The two more frequent hereditary cancer syndromes are Hereditary Breast and Ovarian Cancer and Hereditary Colorectal Cancer.
It is important to identify families with hereditary cancer and their specific mutation, because genetic testing can identify which family members are at higher risk and which are not. This information can then be used to personalize options for early detection (screening programs) or prevention of cancer.
Hereditary Breast and Ovarian cancer (HBOC)
Most breast tumors are defined as “sporadic” tumors, as they occur in women without a significant family history of this pathology. A minority of cases, about 15%, are instead defined as “familial” tumors, since in each nucleus of these families there is more than one affected component. Finally, about 5-10% of breast tumors are considered “hereditary”, in other words attributable to the presence of constitutive variants in DNA that confer a much higher risk of tumor development than the general population. However, the development of the pathology depends on the interaction of various factors: hormonal, metabolic, environmental and genetic.
The main susceptibility genes, BRCA1 and BRCA2, are associated with about 15-20% of hereditary breast cancer cases and about 10-15% of hereditary ovarian cancer cases.
For more information on HBOC, click here.
Hereditary Colorectal Cancer
Colorectal cancer occur in about 5-6% of individuals in the general population. In some rare cases (5-10%) these tumors are due to the presence of an inherited genetic predisposition to the development of tumors. The most frequent forms of inherited predisposition to the development of colorectal cancer are Lynch Syndrome, due to alterations in the MLH1, MSH2, MSH6, PMS2, EPCAM genes and Familial Polyposis, caused mainly by mutations in the APC and MUTYH genes.
For more information on Hereditary Colorectal Cancer, click here.
What is personalized therapy?
Personalized therapy is a term to describe a medical care which is based on the presence of a pathogenic variant in one’s genes and on the specific disease. The choice of a given therapy will be based on the fact whether a given pathogenic variant is present in one’s genes or not. To address this question a molecular analysis is performed on a tissue sample from the tumor. Personalized therapy sometimes is also called personalized medicine or precision medicine.
For example, cancer patients that carry a hereditary pathogenic variant in BRCA1or BRCA2 or that have a spontaneously acquired pathogenic variant in either of the two genes in the tumor, might be eligible for treatment with a specific agent called Olaparib.
How is genetic testing performed?
Genetic testing is done by analyzing small samples of blood, saliva, or tissue to look for changes in genes or chromosomes.
- DNA will be extracted from the sample that has been send for analysis.
- After extraction, the DNA will be sequenced which means that the single bases of the genes of interest will be read and analyzed to identify any potential pathogenic variants.
- A laboratory genetics will read and interpret the result.
- The final report will be sent to the treating doctor or to medical genetics who ordered the test.
- They will discuss the results with the patient and explain the implications of the findings for him and his family.
How to access testing?
ASST Garda - Ospedale di Desenzano del Garda
ASST Garda - Ospedale di Manerbio
ASST Lariana - Ospedale S.Anna
ASST Lecco – Ospedale Alessandro Manzoni
ASST Mantova - Ospedale Carlo Poma
ASST Settelaghi - Ospedale di Circolo
Visualizza Ospedali convenzionati Cogentech in una mappa di dimensioni maggiori
For patients
Testing can only be performed in the contest of genetic counseling. We recommend that you talk to you doctor if you suspect to have a family history of tumors. He will refer you to medical genetics for further anamnesis to decide whether testing is indicated.
For doctors and hospitals
Cogentech provides genetic testing in collaboration with hospitals.
If you are interested in stipulating a collaboration, please contact us for further details.
SSN Accreditation
Cogentech's genetic testing laboratory is officially accredited with the National Health Service (SSN) with registration in the Regional Registry of Accredited Facilities at No. 1118 on 08/31/2011 in the sub-branch of Cytogenetics and Medical Genetics for specialized laboratory services in Genetics and Molecular Biology.

